In Vitro Fertilization
IVF, or In Vitro Fertilization, is a series of procedures to assist women with fertility or genetic conditions in conceiving a child. It is also commonly used in the surrogacy process.
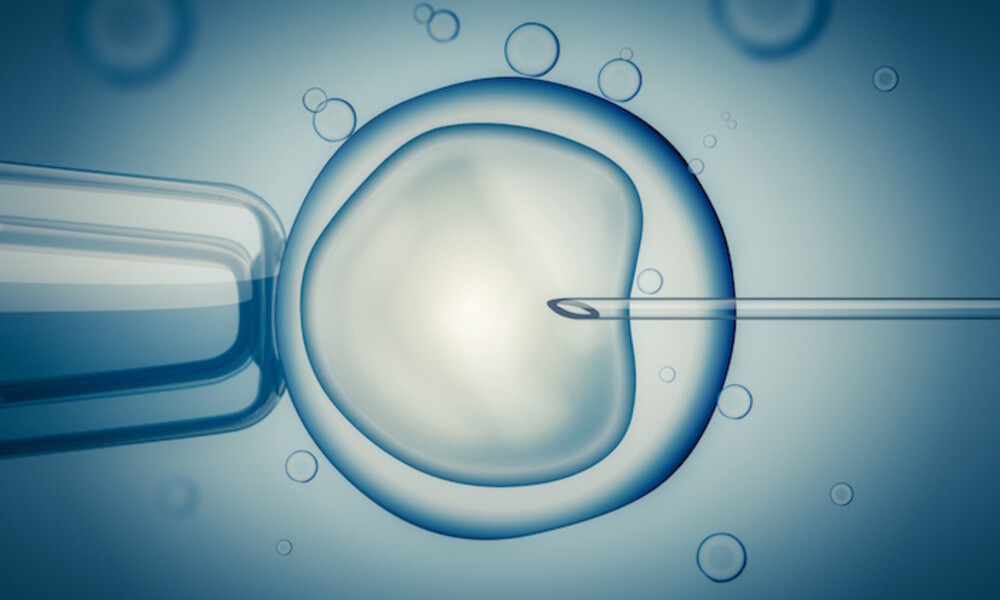
In natural conception, an egg is fertilized by the sperm inside the woman’s body and attaches to the lining of the womb where conception starts. IVF is an assisted reproductive technology (ART), technology that helps a woman achieve pregnancy, that involves removing a woman’s egg from her body and combining it with a man’s sperm to create an embryo. “In vitro” means “in glass” where the egg and sperm are artificially fertilized in a laboratory dish instead of inside a woman’s body.
A woman consults a reproductive endocrinologist, one who specializes in infertility, and undergoes several tests before being referred to try out IVF. Once IVF is suggested, the woman is prescribed to take fertility drugs or hormones to prepare her reproductive organs for conception.
The embryo formed is then artificially inseminated into the woman’s uterus where the woman waits for signs of conception.
IVF in Numbers
In 2013, nearly 63,000 infants were born with the help of IVF. According to the report from the Society for Assisted Reproductive Technology, babies conceived through fertility treatments account for more than 1.5 percent of children born in the United States out of the 3 million born every year.
One IVF cycle does not guarantee immediate conception. Many patients think that an excellent IVF success rate is 80% or above, and that anything below 50% is poor. Well, did you know that even a young and fertile couple has just a 15-20% chance to conceive naturally in any one month? Women with top chances of IVF success have per-cycle success rates of 40% or higher, while the majority of women have per-cycle success rates of 20-35%. Having this perspective may help you think about trying more than one cycle, and feel less discouraged if the first one doesn’t work.
Embryo Transfers
Embryo transfer is the final step of the IVF process. Single embryo transfers are the industry standard and have proven better outcomes for both baby and surrogate. Why? There have been major strides in medical and genetic testing of embryos, ensuring the most viable embryo is selected for transfer which not only increases the success rate of a full term, healthy delivery. It also lowers the medical risks associated with carrying multiples to both the surrogate and the fetus.
After the eggs are fertilized with the sperm to create an embryo, the highest quality embryo is transferred to the woman’s uterus in hopes that it will implant into the lining and begin to grow.
The embryo is then loaded into a fine transfer catheter that is inserted into the vagina to reach the uterus.
An embryo may be transferred anytime between the first to the sixth day after the egg is retrieved, however some clinics are now allowing the embryo to reach the blastocysts stage before the transfer, which occurs around day five.
The procedure does not require anesthesia, although a sedative is often used. For most women it is a completely painless process, although there are a few patients that experience mild cramps after the procedure.
After the procedure, the woman is prescribed to take more progesterone to ensure her body responds to the conception process and to help sustain pregnancy. It is discontinued once the pregnancy has been confirmed and the body is able to produce progesterone on its own.
The IVF Process
There are five basic steps to IVF:
Step 1: Stimulation of the Ovaries
Fertility drugs are given to boost the ovaries’ egg production. Without fertility drugs, once a month, a woman will naturally produce one egg. However, with the assistance of fertility drugs, the egg production goes into overdrive and produces multiple.
Once the woman is on regular hormones, she will undergo regular transvaginal ultrasounds to check the ovaries, and blood tests to check hormone levels.
Step 2: Removing the Egg
Retrieval of the egg is usually done in the doctor’s office as an outpatient procedure. The woman will be given sedatives to make the process painless. A thin needle is inserted through the vagina to reach the eggs inside the ovaries and extract them using a suction device.
This process is generally done on both ovaries. There may be some cramping felt after the procedure, but most women don’t feel it. Usually if there is any cramping, it will go away within a day.
In rare cases, a pelvic laparoscopy is recommended to extract the eggs. This is when several attempts through the outpatient process fails. If a woman is infertile or acts as a surrogate, eggs can be from a donor or intended parents.
Step 3: Insemination and Fertilization
A man’s sperm and a woman’s best eggs are mixed together in a dish. This process is called insemination. It is stored in a chamber with a controlled environment where the eggs and the sperm are given the chance to incubate.
If the sperm count is low, the chances of fertilization through mixing decreases. Instead, intracytoplasmic sperm injection (ICSI) is performed. This is done by directly injecting the sperm into the egg to ensure that the egg fertilizes.
Step 4: Embryo Culture
Once the egg is fertilized, it becomes an embryo within five days. During this stage, a Preimplantation Genetic Diagnosis (PGD) is recommended to diagnose a genetic disorder in early embryos prior to implantation and pregnancy. It is done 3 – 4 days after fertilization.
Through PGD, parents are able to choose which embryo to implant. The procedure is typically used to:
Screen out embryos carrying a genetic disease
Predict the risk of disease
Improve birth rates of healthy babies following ART
Step 5: Embryo Transfer
Embryos are implanted into the woman’s uterus after an embryo culture is formed. This usually takes 3 – 5 days after the eggs were removed for fertilization. It is an outpatient procedure usually done in the doctor’s office.
During the process, a catheter containing the embryos is inserted into the woman’s vagina towards the uterus, to implant the chosen embryo. Patients can opt to freeze unused embryos to use or donate in the future.
Post IVF
Rest is recommended after the embryo transfer to ensure that the embryo sticks to the wall of the uterus. Complete bed rest is highly recommended to women with increased risk of Ovarian Hyperstimulation Syndrome (OHSS) or swollen ovaries.
The recipient is usually prescribed to continue on progesterone for 8 – 10 weeks after the embryo transfer. It helps thicken the uterus making it easier for the embryo to implant. After 2 weeks, she will be asked to return to the clinic and undergo a pregnancy test to ensure that the IVF process was successful. Once proven successful, the embryo will continue to grow in the same way as if in natural conception.
As with any pregnancy the surrogate should maintain regular scheduled check ups with her OB/GYN to ensure that the baby is developing properly and her body is not strained. Then, all that’s left is to prepare for the baby’s birth and await its arrival.
Other Symptoms
If you or someone you love has just received IVF and experiences any of the symptoms below, call your healthcare provider right away:
- A fever over 100.5 F (38 C)
- Pelvic pain
- Heavy bleeding from the vagina
- Blood in the urine
IVF can seem like an intimidating process at first, with lots of steps and testing, but when completed results in the most miraculous of occurrences. It is only through IVF that couples struggling to have families of their own can have children genetically their own without actually getting pregnant themselves. And of course this could not be done without the generosity of surrogates who lend their bodies to this process. IVF gives couples another chance and ultimately makes all the effort worth it in the end.
To find out more about how you can become a surrogate for ConceiveAbilities, read our page How To Become A Surrogate.
To find out more news, guides, and events related to surrogacy, be sure to visit our blog!